Malaria treatment
Myanmar has the highest malaria burden in South-east Asia. Malaria transmission is largely concentrated in remote and hard to reach communities.
These communities are small and far apart, with a poor infrastructure. There are no trained health professionals in these communities. MAM started malaria activities in 2011 by training villagers to use a rapid diagnostic test for malaria and to provide treatment in their community. This has been very successful.


Between 2011 and 2020 MAM trained 2,447 Village Health Workers (VHWs), who tested 1,579,104 patients for malaria and treated 63,715 patients with confirmed malaria.
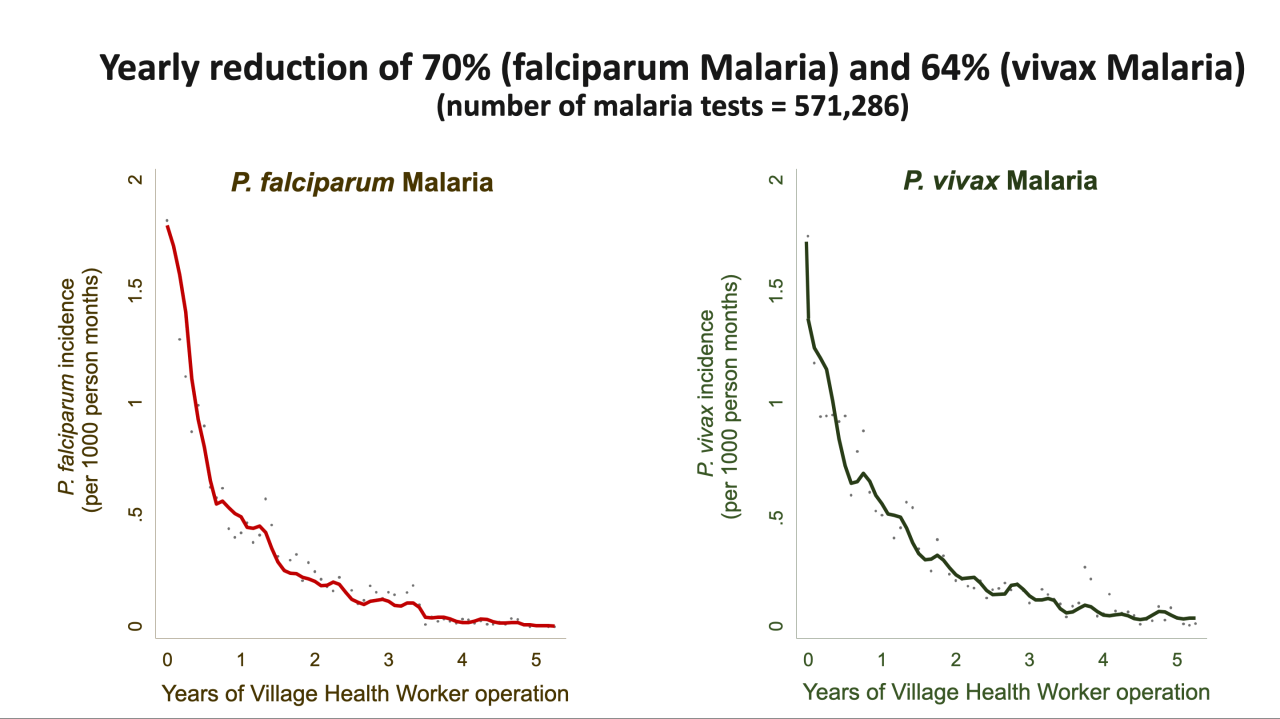
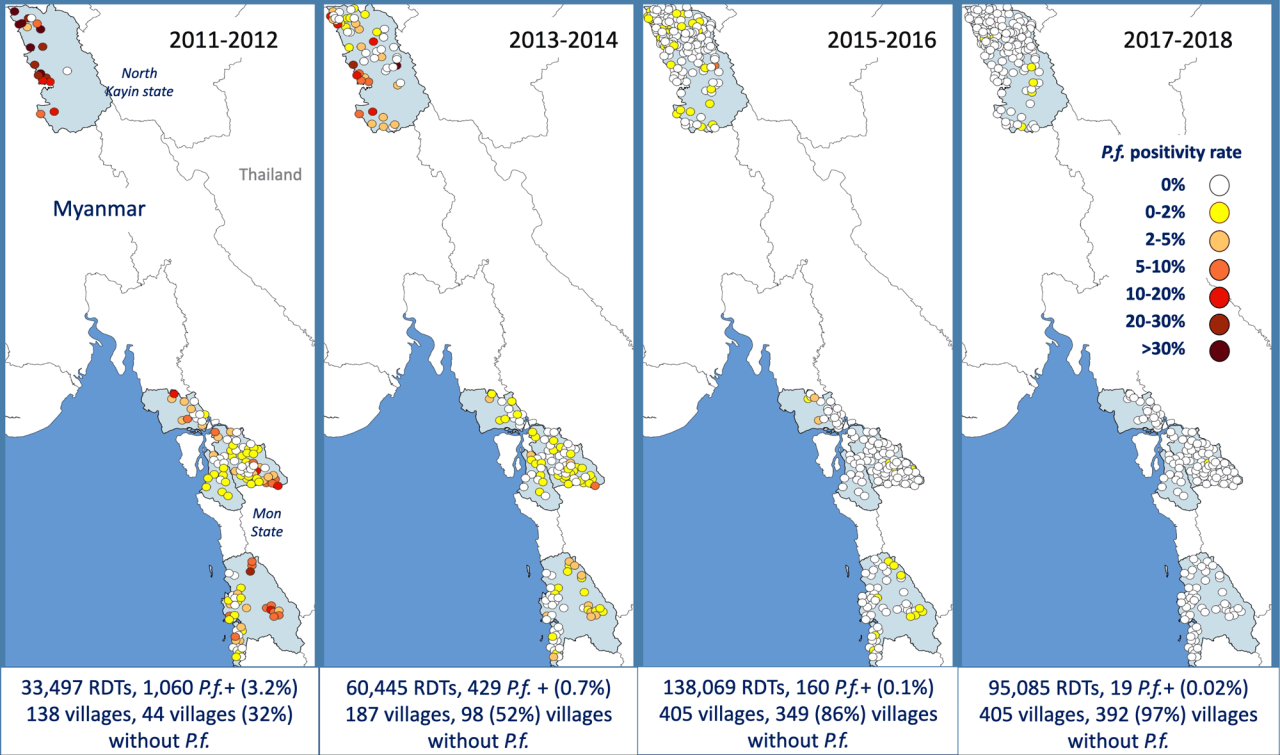
67% of these cases had falciparum malaria, a species that causes a severe form of malaria. In addition the VHWs distributed 588,617 impregnated mosquito-nets. After introduction of the Village Health Workers malaria decreased rapidly and completely disappeared in most villages (figure).

Malaria is the leading cause of morbidity and mortality in Myanmar.
Malaria cases are estimated at 4-8 million per year (although it is believed that the incidence has decreased over the past years). and malaria deaths are estimated at 9,097 while others believe that it can be as high as 40,000 to 80,000 per year.
Malaria management in Myanmar is inadequate. Lack of good diagnostics and consequent empirical clinical diagnosis based on non-specific symptoms is still common practice. Cheap, ineffective and/or incomplete anti-malaria treatments are still commonly prescribed. Fake medicines are sold widely.

Artemisinin derivates are a ‘new’ (+/- 30 years) class of highly effective anti-malarials and artemisinin-based combination therapy (ACT) [artemisinin + another antimalarial drug] is now considered as the best treatment for falciparum malaria and recommended throughout the world.
Replacing ineffective regimen with ACT has significantly reduced morbidity and mortality. In 2008 artemisinin resistance was identified in Western Cambodia.
Exposure to incomplete treatment for many years has probably been the driving force in the selection of resistant parasites. Subsequent monitoring in the region discovered that artemisinin resistance is also present on the Chinese- Myanmar (Kachin) border and on the Myanmar-Thai border (Kayin, Mon and Tanintharyi provinces).

